Lymphokine-Activated Killer Cell (LAK) Thearpy
Boosting Lymphocytes to Strengthen Immunity
Lymphokine-Activated Killer (LAK) cell therapy, also known as killer T-cell therapy, involves extracting lymphocytes from the patient’s blood, activating and multiplying them to over a thousand times their original count (reaching approximately five billion cells) in a laboratory setting, and then reintroducing those cells into the patient via infusion. By substantially enhancing the body’s immune response, LAK therapy equips patients to combat various cancers. In Japan, physicians often refer to this amplification of immune cells simply as LAK (lymphokine-activated killer cell) therapy.

The “Killer T-Cells” Within Lymphocytes
Killer T-cells (Cytotoxic T Lymphocytes) are a critical subset of lymphocytes that actively target and destroy cells infected by viruses or harboring genetic mutations. They identify “abnormal” cells by detecting specific proteins (antigens) on the cell’s surface, then use a syringe-like mechanism to inject cytotoxic agents, causing the cells’ membrane to rupture. Killer T-cells also release cytokines (e.g., interferons, interleukins) to help other immune cells mount a coordinated defense. Thus, they serve as a crucial frontline in the fight against cancer cells.
Why Is LAK Therapy Necessary?
When confronted with cancer cells, the body requires an immediate surge of lymphocytes to launch an effective assault. Relying solely on the body’s natural proliferation often fails to keep pace with rapidly spreading cancer cells. By culturing and activating lymphocytes outside the body, LAK therapy provides an infusion of “elite reinforcements,” quickly elevating the immune system’s capacity to target and eliminate malignancies.

The Key Role of Lymphocytes
In human blood, immune cells break down roughly as follows:
1. Neutrophils (~70%): Primarily combat bacterial infections. If neutrophils drop below 1,500/μL, the risk of sepsis soars.
2. Lymphocytes (~25%): Contain killer T cells, B cells, and NK (natural killer) cells, crucial for fighting viruses and abnormal cells.
3. Monocytes: Collaborate with other immune mechanisms to fend off pathogens.
4. Eosinophils and Basophils: Though they make up a small percentage, they still serve specialized functions in allergic reactions and certain infections.
When lymphocytes are low, the body lacks an effective offense against powerful adversaries such as malignant tumors. LAK therapy addresses this shortfall by quickly multiplying lymphocytes, ensuring the immune system regains its strength.
Consequences of Insufficient Lymphocytes
1. Reduced Defense: A deficiency in lymphocytes makes it easier for cancer cells to spread, exacerbating the disease.
2. Recurrent Infections: The weakened immune system also struggles to fend off bacterial or viral infections, leading to complications such as pneumonia or gastrointestinal infections.
Common Causes of Low Lymphocyte Counts
1. Cancer Itself: Cancer patients typically have immune activity around 30% lower than average.
2. Chemotherapy or Radiotherapy: These treatments significantly lower lymphocyte counts.
3. Physical and Emotional Stress: Surgery, fatigue, pain, and anxiety can all reduce lymphocyte activity.
4. Metastasis or Recurrence: If cancer has spread to organs like the liver, lungs, or peritoneum—or if local recurrence occurs—lymphocyte activity often drops to about half that of a healthy individual.
How To Check Your Lymphocyte Counts?
A WBC (White Blood Cell) count and microscopic blood analysis can give a preliminary overview of your immune cell status:
1. A typical lymphocyte count should range from roughly 1,000 to 1,500 cells/μL.
2. If the count falls under 1,000 cells/μL, fatigue and recurrent infections (e.g., pneumonia, enteritis) may occur.
3. Below 500 cells/μL is considered an immunodeficiency state, placing patients at high risk for aggressive tumor growth and severe infections.
One main objective of LAK therapy is to maintain a lymphocyte count above 1,500 cells/μL, thus ensuring sufficient immune support to contain cancer growth.

LAK Therapy Procedure and Side Effects
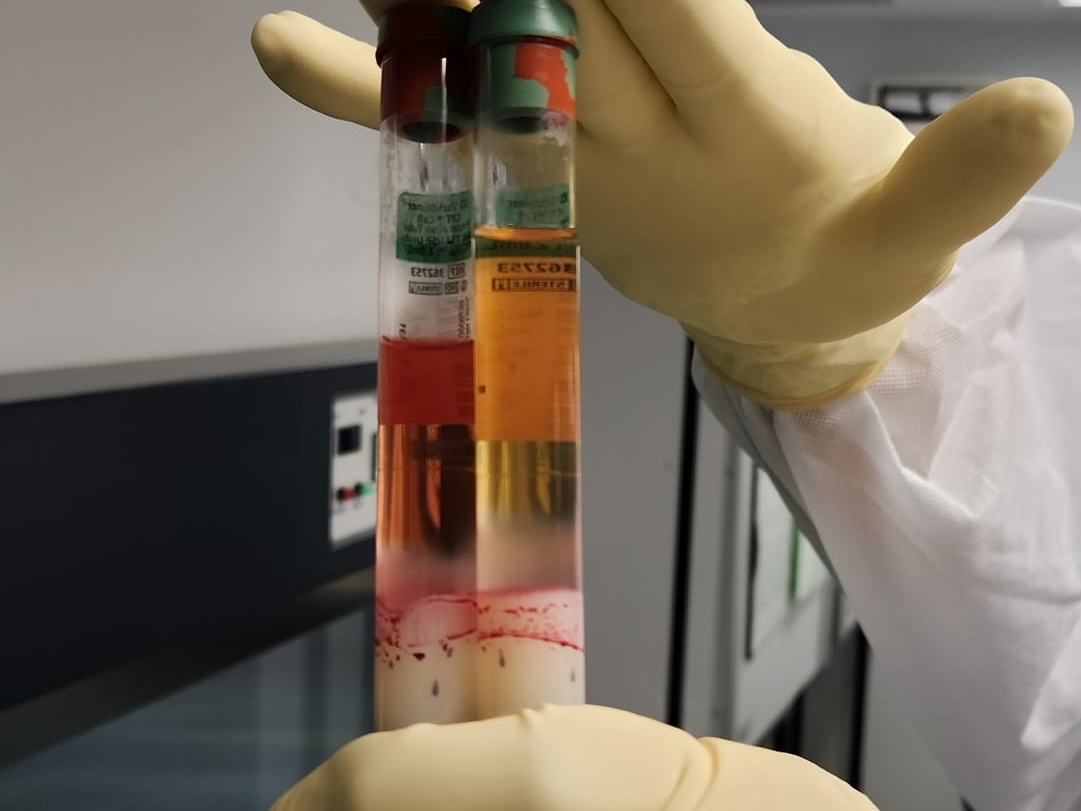
1. Blood Collection and Separation
The doctor first collects two blood samples from the patient, each containing 7cc. The samples are then processed in the laboratory to isolate lymphocytes.
2. Artificial Activation and Large-Scale Proliferation
The lymphocytes are then cultured in a controlled environment and treated with growth factors to amplify their numbers—resulting in a “burst” of power from just thousands to several billion cells in a short span.
3. Reinfusion into the Body
These cultivated lymphocytes are infused back into the patient, quickly filling in any immune deficits and assisting in the fight against cancer cells.
Side Effects
Because LAK therapy uses the patient’s own immune cells, side effects are relatively mild. A small percentage of patients may develop a low-grade fever within 1–2 days of infusion; symptoms typically subside within a few hours to half a day. Clinic keeps antipyretics on hand and recommend rest to mitigate any discomfort.
Where Can You Receive LAK Therapy?
At the Shin-Yokohama Kato Clinic in Tokyo–Yokohama, Clinic Director Dr. Yoichi Kato has over 20 years of experience in immunocellular therapies and a track record of more than 2,000 clinical immunotherapy cases—making him one of Japan’s most accomplished specialists in the field. Patients contemplating treatment in Japan can begin with an online consultation so that Dr. Kato can review their medical records and overall condition, then determine eligibility for LAK therapy and develop a personalized treatment plan.
![加藤洋一博士(Dr. Yoichi Kato)[3].jpg](/uploads/image/202502/%E5%8A%A0%E8%97%A4%E6%B4%8B%E4%B8%80%E5%8D%9A%E5%A3%AB(Dr.%20Yoichi%20Kato)[3].jpg)
Dr. Yoichi Kato
As a trusted partner of Dr. Kato, Asia Immunotherapy provides comprehensive support services, including:
1. Collecting and compiling medical reports.
2. Arranging online consultations with Dr. Kato.
3. Coordinating travel and accommodation in Japan.
4. Offering airport pick-up and professional interpretation throughout the treatment period.
Through detailed planning and thorough logistics, we help patients receive immunocellular therapy in Japan safely and securely—taking a critical step in the fight against cancer.
Asia Immunotherapy - Central, Hong Kong
Lymphokine Activated Killer Cells & Natural Killer Cells Lymphocytes in Immunotherapy
Explore the roles of lymphokine activated killer cells and natural killer cells lymphocytes in cancer treatment. Learn how these immune cells function in cellular immunotherapy protocols.
LAK Cell Therapy: Boosting Your Immune System with Lymphokine-Activated Killer Cells
LAK Cell Therapy (Lymphokine-Activated Killer Cell Therapy) is an advanced form of autologous cell treatment designed to significantly amplify the body's natural defense mechanisms. This therapy is rooted in using the patient’s own immune cells—specifically lymphokine activated killer cells—which are cultured and activated in a specialized environment before being returned to the body.
Widely utilized in Japan, LAK Therapy is highly effective at enhancing the body's protective cells against cancer and viral threats. It works by creating a powerful, non-specific anti-cancer army, making it a valuable component in a personalized, multi-modal treatment strategy.
Core Function:
- Mechanism: Utilizes the patient’s own lymphocytes, massively expanded outside the body.
- Primary Role: To augment the body’s non-specific defenses, offering broad-spectrum capacity against malignant cells.
- Application: Often used in combination with other targeted immunotherapies or conventional treatments.
The Science Behind Lymphokine-Activated Killer Cells
The term lymphokine activated killer cells defines a heterogeneous group of immune cells that have been given a significant boost in their anti-cancer efficacy through laboratory methods. This transformation is driven by specialized biological messengers.
Activation Through Lymphokines
The therapy begins by extracting lymphocytes—the protective white blood cells—from the patient’s peripheral blood. These cells are then immersed in a culture medium containing high concentrations of lymphokines, most notably Interleukin-2 (IL-2). This potent stimulation causes the lymphocytes to proliferate rapidly, yielding a massive quantity of highly aggressive LAK cells, dramatically enhancing their ability to seek and destroy abnormal cells.
The Cellular Composition of LAK
The resulting LAK cell population is a powerful composite, containing highly activated forms of various protective cells, including T-lymphocytes, B-lymphocytes, and crucially, Natural Killer (NK) cells.
LAK Cells and Their Relationship with Natural Killer Cells Lymphocytes
Understanding the interplay between LAK cells and natural killer cells lymphocytes is key to appreciating this therapy's power. NK cells are a major component and the primary engine of the LAK response.
The Role of NK Cells within the LAK Group
- NK Cell Identity: Natural Killer (NK) cells are themselves a type of lymphocyte and a critical part of the innate (first-line) immune system. They possess the unique ability to recognize and kill cancer cells and virus-infected cells without prior sensitization.
- LAK Enhancement: The lymphokine activation process significantly boosts the number and cytotoxicity (killing power) of the NK cells present within the LAK cell group. These highly active NK cells are a major source of the non-specific, broad-spectrum anti-cancer effect associated with LAK therapy.
- Synergistic Attack: The LAK cell population provides a synergistic effect—the NK cells launch their non-specific, immediate attack, while the T-cells and other lymphocytes in the mix contribute to a broader, comprehensive immune response against cancer.
The LAK Therapy Process at Asia Immunotherapy
Our commitment to excellence, overseen by Dr. Yoichi Kato's expertise, ensures a safe and effective therapeutic journey for our international patients, including those from Canada.
- Blood Collection: A simple blood drawing procedure is used to collect the necessary lymphocytes.
- Culture and Expansion: In the controlled environment of the Shin-Yokohama Kato Clinic's laboratory, the lymphocytes are rapidly multiplied—often by more than a thousandfold—and activated using specialized lymphokines.
- Infusion: The dramatically increased population of potent LAK cells is returned to the patient’s bloodstream via an IV drip.
- Safety and Monitoring: Throughout the treatment and post-infusion phase, patients receive professional care and monitoring to track their immune response and ensure safety.
Benefits and Strategic Applications of LAK Cell Therapy
LAK Therapy is a strategic option in oncology, particularly when used in combination with other treatments:
- Broad-Spectrum Anti-Cancer Capacity: The non-specific killing mechanism targets a wide variety of malignant cells, providing a robust general defense.
- Immunological Synergy: LAK therapy combines effectively with other advanced protocols, such as DC vaccines or NK cell therapy, to achieve a more comprehensive and layered anti-cancer attack.
- Improved Immune Function: The massive expansion of protective cells provides a significant temporary boost to the patient’s overall immune competence.
Explore Your Personalized Immune Strategy
If you are exploring ways to significantly strengthen your body's anti-cancer immunity, LAK Cell Therapy may be a key component of your personalized plan. Contact us to consult with our specialized team.
Contact our International Patient Coordinator:
- Tel / WhatsApp: +852 3480 8393
- Email: info@asiaimmune.com
Recommended reading
Enhancing Dendritic Cell Therapy in Solid Tumors with Immunomodulating Conventional Treatment_臨床醫學報告_新聞及臨床報告_亞洲免疫治療
Dendriticcells(DCs)arethemostpotentantigen-presentingcellsandarethekeyinitiatoroftumor-specificimmuneresponses.ThesecharacteristicsareexploitedbyDCtherapy,whereDCsareexvivoloadedwithtumor-associatedan
What are Dendritic Cells?_新聞_新聞及臨床報告_亞洲免疫治療
Dendriticcellsareatypeofantigen-presentingcell(APC)thatformanimportantroleintheadaptiveimmunesystem.Themainfunctionofdendriticcellsistopresentantigensandthecellsarethereforesometimesreferredtoas“profe
Targeting dendritic cells in pancreatic ductal adenocarcinoma_臨床醫學報告_新聞及臨床報告_亞洲免疫治療
Dendriticcells(DC)areanintegralpartofthetumormicroenvironment.PancreaticcancerischaracterizedbyreducednumberandfunctionofDCs,whichimpactsantigenpresentationandcontributestoimmunetolerance.


